Vascular Neurology Fellowship
Mission Statement
The Vascular Neurology rotation provides residents with the knowledge and skills to diagnose, manage, and prevent cerebrovascular diseases. Our mission is to train residents in evidence-based, patient-centered care for patients with stroke and other vascular neurologic conditions while emphasizing rapid intervention, multidisciplinary collaboration, and long-term recovery planning.
Educational Level & Duration
- PGY-2: 1 month
- PGY-3: 1 month
Goals
The rotation prepares residents to:
- Recognize and manage acute ischemic stroke, hemorrhagic stroke, and transient ischemic attacks.
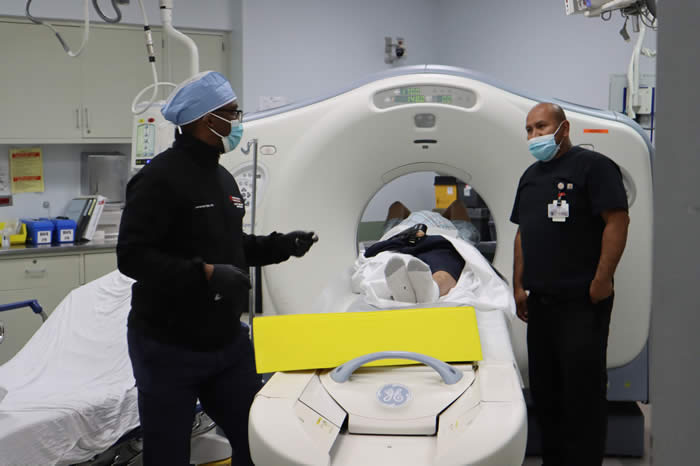
- Apply appropriate diagnostic studies, including CT, MRI, MRA, CTA, and vascular ultrasound.
- Participate in the evaluation and initiation of acute stroke therapies, including thrombolysis and mechanical thrombectomy.
- Understand secondary prevention strategies and rehabilitation planning for stroke patients.
Objectives
Residents are expected to:
- Perform a focused neurologic exam in patients with suspected stroke.
- Interpret neuroimaging and vascular studies for diagnosis and management.
- Initiate acute management of ischemic stroke including IV tPA protocols.
- Assist in patient selection and preparation for mechanical thrombectomy.
- Manage complications of acute stroke such as increased intracranial pressure, hemorrhagic conversion, and seizures.
- Develop discharge and rehabilitation plans with appropriate referrals.
- Provide counseling on stroke risk factors and preventive strategies.
Assessment & Feedback
- Daily faculty assessment through direct observation.
- Formal evaluation upon completion of the rotation.
- Feedback on diagnostic accuracy, clinical judgment, procedural skills, and communication with patients and families.
Educational Structure & Curriculum
Rotations Include:
- Neurocritical Care & Consult Service (Acute Inpatient Stroke)
- Interventional Neurology (Neurointerventional Surgery)
- Electives: Neuroimaging, Neurorehabilitation, Behavioral Neurology, Child Neurology, Clinical Neurophysiology, Neurogenetics, Neuromuscular Medicine, Neuro-oncology, Neuro-ophthalmology, Neuropathology, Pain Management, Psychiatry, Sleep Disorders.
Didactics
- Weekly Board Review sessions (fellows must present at least once a month).
- Morning Report (Wednesdays).
- Journal Club (preassigned; fellows lead discussions).
- Morbidity & Mortality Conference (quarterly).
- Grand Rounds (quarterly).
- Quality Improvement meetings (quarterly).
- Tumor Board (optional, twice monthly).
- In-Service Exam (RITE – February, mandatory).
Clinic
- Outpatient continuity clinic with vascular neurology faculty.
- Fellows must log all clinic patients in New Innovations.
Competencies & Training Focus
Fellows are trained under the ACGME Core Competencies:
- Professionalism
- Patient Care & Procedural Skills
- Medical Knowledge
- Practice-Based Learning & Improvement
- Interpersonal & Communication Skills
- Systems-Based Practice
Training Emphasizes
- Code Stroke management and acute neurovascular care.
- Supervision progression: fellows gain conditional independence after approximately three months.
- Participation in the Stroke Committee and Quality Improvement (QI) initiatives.
- Fatigue management, wellness, and professionalism standards.
Evaluation & Oversight
- Formative: ongoing feedback from faculty.
- Milestones: semi-annual evaluations by the Clinical Competency Committee (CCC).
- Summative: end-of-rotation, annual, and final program evaluation.
- Faculty & Program Evaluations: fellows provide anonymous evaluations; Annual Program Evaluation conducted by the Program Evaluation Committee (PEC).
Fellow Expectations
- Attendance: minimum 80% required for didactics.
- Work Hours: capped at 80 hours per week, with required time off per ACGME rules.
- Participation in research, scholarly activity, or presentations required.
- Must attend at least one professional conference (regional, national, or international).
Curriculum
Placeholder….
